Parathyroid Disease
What is Parathyroid Disease?
The parathyroid glands normally produce a substance called parathyroid hormone ( PTH). PTH plays a critical role in the regulation and metabolism of calcium within the body. Normally this is under tight regulation from various feedback mechanisms within the body.
When the Parathyroid glands do not function correctly it is mostly associated with disorders related to either overactive or underactive gland secretions.
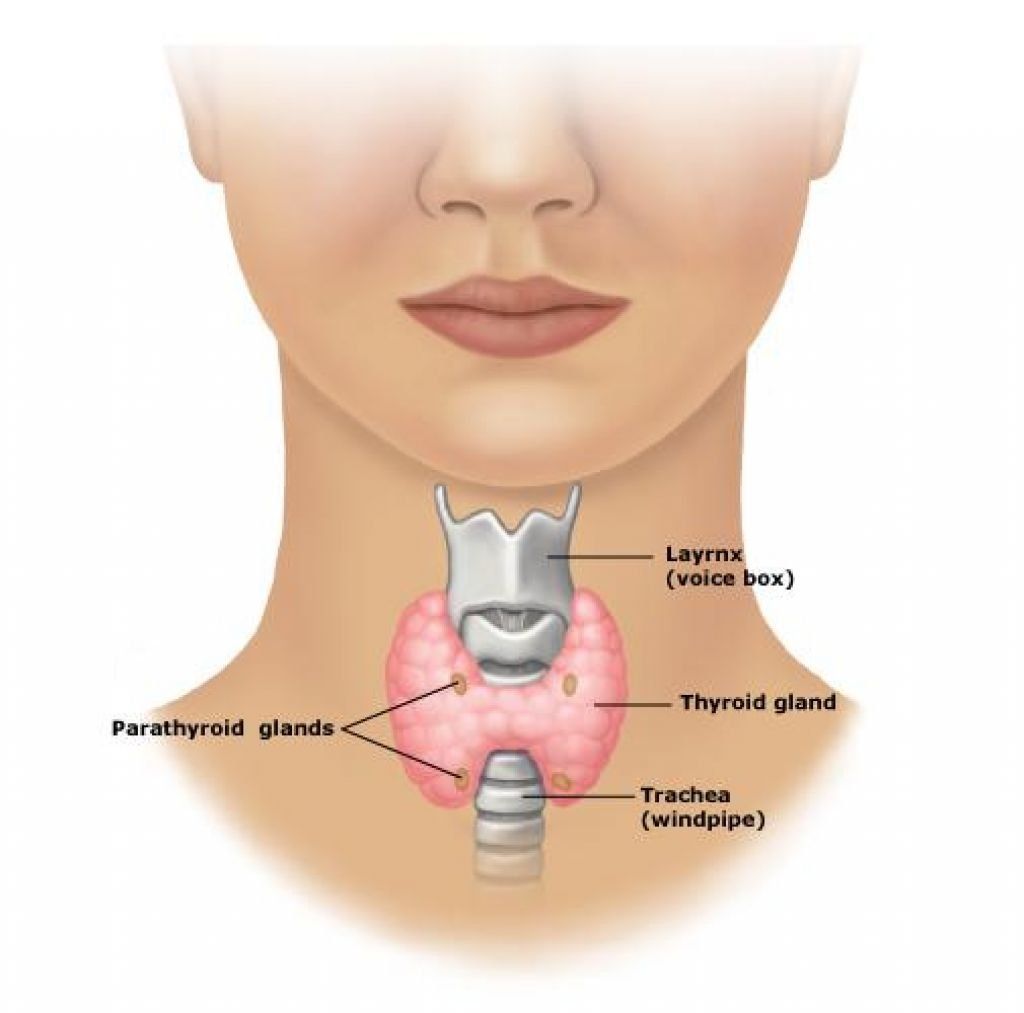
What is the Anatomy of Parathyroid Glands?
There are four ‘pea sized’ lobes or glands that are located usually immediately behind the thyroid in your neck adjacent the Trachea (windpipe). ‘Para’ means ‘near’, which explains the name.
While the Parathyroid glands are part of the body's endocrine system, the thyroid and parathyroid glands are completely different. The endocrine system consists of a range of glands that secrete hormones into the bloodstream.
What hormones help regulate calcium and phosphate?
- Parathyroid Hormone (PTH)
- Vitamins D
- Calcitonin
- FGF-23
The main parathyroid hormone (PTH) is a chemical that regulates the amount of calcium, phosphorus and magnesium in the bones and blood.
What is the Impact of Parathyroid Disease
The minerals calcium and phosphorus are crucial for healthy bones. Blood-borne calcium is also needed for the proper functioning of muscle and nerve cells.
Every cell and organ in the body uses calcium as a signal to regulate their normal function. Therefore, it is crucial that calcium levels are tightly controlled.
What are the Types of Parathyroid Disease
Hyperparathyroidism
Causing abnormally high blood calcium levels (hypercalcaemia) occurs when the Parathyroid gland releases extra PTH, mainly "stealing" calcium from the bone.
This condition can lead to:
- Abdominal pain
- Kidney stones
- Osteoporosis and fractures
- Mood disturbances and fatigue
- Pancreatitis (inflammation of the pancreas)
In severe elevations of blood calcium levels called "hypercalcemic crisis," a patient can become comatose or near-comatose due to organ failure.
Hypoparathyroidism
Hypoparathyroidism is characterised by low levels of PTH, this causes glands to drop hormone production, which decreases the amount of calcium in the blood. This then affects nerve and muscle cells which are unable to function properly.
Hypoparathyroidism can cause:
- Teeth fail to form or be slow to emerge
- Impair mental development
- Addison’s disease and
- dysmenorrhoea (painful menstrual periods)
Multiple Endocrine Neoplasia 1
Multiple endocrine neoplasias 1 (MEN1) is an inherited condition, characterised by tumours on at least two glands of the endocrine system.
MEN1 can involve tumours in the parathyroid glands and any other hormone producing organs including the pituitary, pancreas, adrenals and thyroid.
Who are is at Risk of Parathyroid Disease
Parathyroid Disease commonly affects more women aged 50 years and over. The most common age to be diagnosed with Parathyroid disease is the early 60's with most sufferers between 40 and 75.
Patients in this group may also have heart problems related to the high calcium.
Other ages also get parathyroid disease, but in younger patients, it is typically due to a genetic/family disorder such as MEN-1 syndrome.
What are the Causes of Parathyroid Disease
Hyperparathyroidism can be caused by:
- a small tumour (adenoma) in the gland.
- chronic kidney (renal) disease
- particular medications, such as anticonvulsant drugs
Hypoparathyroidism can be caused by:
- magnesium deficiency,
- injury to the glands,
- surgery on the nearby thyroid gland,
- genetic disorder or
- the congenital lack of parathyroid glands.
Hypocalcaemia can be caused by a lack of vitamin D
Multiple endocrine neoplasias 1 is a genetic disorder
What Symptoms of Parathyroid Disease
Symptoms of Hyperparathyroidism may include:
- Pain in the bones and joints
- Increased susceptibility to bone fractures
- Shrinking height
- Backache
- Muscle aches
- Thirst
- Frequent urination
- Abdominal pain
- Fatigue
- Nausea
- Loss of appetite
- Depression and other personality changes.
Symptoms of hypoparathyroidism may include:
- Pins and needles
- Brittle hair and nails
- Dry, roughened skin
- Muscle cramps and spasms
- Convulsions.
Symptoms of Multiple Endocrine Neoplasia 1 may include:
- Nausea, vomiting, black faeces
- Abdominal pain,
- Persistent indigestion and bloating.
- Vision problems.
- Weight loss.
- Hypotension (low blood pressure).
- Reduced sex drive.
These symptoms depend on which glands are affected.
How is Parathyroid Disease Diagnosed
Patients are diagnosed through routine blood testing or screening for osteoporosis and many patients have only vague, non-specific symptoms.
Hyperparathyroidism
Diagnostic tests for hyperparathyroidism include:
- Pathology to check for calcium, phosphorus, magnesium and PTH levels;
- Nuclear medicine scans or CT scans with contrast to identify where the parathyroid tumour is located
- Ultrasound to localise the tumour and check for thyroid nodules
- Bone density scans and X-Rays
- Renal ultrasound to screen for kidney stones
Hypoparathyroidism
Diagnostic tests for hyperparathyroidism include:
- Pathology to check for calcium, phosphorus, magnesium and PTH levels;
- ECG to check for heart arrhythmia (irregular heartbeat).
Multiple Endocrine Neoplasia 1
Diagnostic tests for Multiple Endocrine Neoplasia include:
- blood tests
- radiology including MRI and CT scans.
What If Parathyroid Disease is Not Treated
If a diagnosis of any Parathyroid disease is made and is not treated it can have serious consequences for the patient’s health.
Depending on the condition untreated Parathyroid disease can lead to worsening symptoms, system failures and premature death.
How is Parathyroid Disease Treated
Hyperparathyroidism
- Thorough investigation to determine the underlying cause. Usually this is due to benign hormone secreting tumour within one of the glands (Parathyroid adenoma)
- Surgery - Parathyroidectomy - Surgical removal of one or more parathyroid glands in the neck.
- Bone health - Helps strengthen and build bones.
- Vitamin - Helps promote normal body function, growth and development.
Hypercalcaemia
- By treating the underlying cause i.e. Excision of parathyroid adenoma
- Dietary restriction of calcium rich foods
- Medications including diuretics, calcium binding agents
- Intravenous fluids and hospital admission in severe cases
Hypocalcaemia
- Dietary supplementation with calcium rich foods
- Calcium tablets
- Vitamin D to promote calcium absorption and retention
- Is usually rare and temporary after parathyroid or thyroid surgery
Multiple Endocrine Neoplasia 1
Treatment varies depending on the combination of glands affected by tumours and their size etc. In the case they are operable or other non-invasive remedies are not suitable treatment can include:
- Mini-parathyroid surgery or
- Parathyroidectomy
When is a Parathyroidectomy Indicated
Parathyroidectomy treatment is indicated for some patients with hyperparathyroidism (high levels of parathyroid hormone) as long term exposure to high blood calcium levels can cause significant health side effects. These include osteoporosis, bone fractures, kidney stones, stomach ulcers and depression.
How is a Parathyroidectomy Performed?
Parathyroidectomy is a surgical procedure that involves the removal of one or more of the parathyroid glands (these glands produce a hormone that increases levels of calcium in the blood).
The type of surgery depends on the type of parathyroid problem and the results of imaging investigations pre-operatively.
Minimally invasive parathyroidectomy: for patients with a single abnormal parathyroid gland that has been identified on imaging this is the approach of choice. It allows exploration of one side of the neck through a smaller incision than is conventionally used.
Gland exploration is the traditional approach to parathyroid surgery that involves a larger incision to allow exploration of both sides of the neck. This is indicated in patients who have hyperparathyroidism without an abnormal gland identified on imaging. It is also used if there is co-existing thyroid disease, in patients with hyperparathyroidism due to renal failure and patients with hereditary parathyroid diseases.
The abnormal gland (tumour) is identified and removed carefully. Sometimes more than one abnormal gland is removed. If all four glands are removed, a part of one of the glands may be implanted in the forearm or the sternocleidomastoid muscle in the neck so that its function is not completely lost.
After removal of the tissue, the incisions are then closed with absorbable hidden sutures and waterproof glue.